World Pneumonia Day observed two days ago highlighted a public health problem of serious concern. With the current weather in Sri Lanka, health officials are concerned that those with flu like symptoms resulting in getting wet in the rain could lead to more serious respiratory diseases such as pneumonia which if not treated in time could leave lasting health complications.
The Sunday Observer asked Consultant Respiratory Physician, National Hospital for Respiratory Diseases, Welisara, Dr Saman Kularatne to explain more about the disease, how it is caused, and how it can be prevented.
Excerpts
Q: As not many readers understand what pneumonia is, as an experienced respiratory physician, describe what it means in layman’s language and the difference between the common flu and pneumonia?
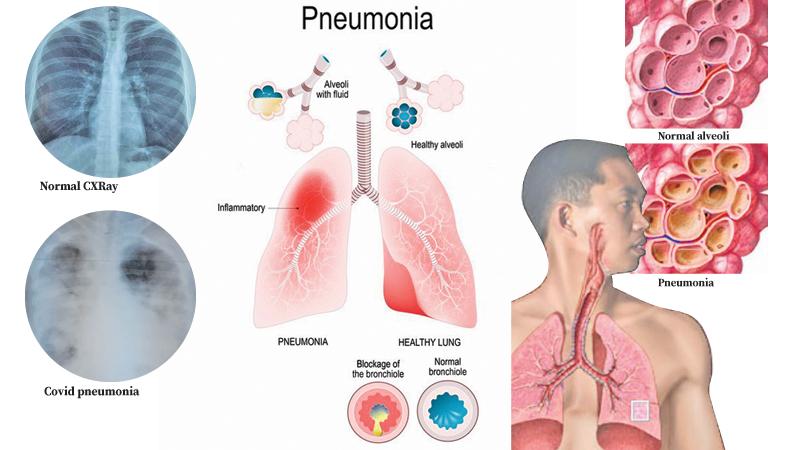
 A: Pneumonia is an infection of the lungs. Our lungs have branching breathing tubes ending up at small air sacs which take oxygen into our body and remove carbon dioxide from the body. Pneumonia is an infection of the lungs. The disease is characterised by inflammation of the lungs primarily affecting the small air sacs known as alveoli.
A: Pneumonia is an infection of the lungs. Our lungs have branching breathing tubes ending up at small air sacs which take oxygen into our body and remove carbon dioxide from the body. Pneumonia is an infection of the lungs. The disease is characterised by inflammation of the lungs primarily affecting the small air sacs known as alveoli.
Influenza viruses cause the flu. The viruses that cause colds may spread more easily in low temperatures. Influenza viruses which cause the flu, may also survive and spread more easily in cold and dry air. Exposure to cold and dry air may also adversely affect the body’s immune system.
Q: What causes it? Studies abroad have indicated that there were over 30 different causes including bacteria, viruses, airborne irritants and fungi?
A: Pneumonia is commonly caused by infection with viruses or bacteria and rarely by other organisms such as fungi. Inhalation or aspiration of irritants also can cause inflammation of the lungs. We use the term pneumonitis for this rather than pneumonia.
Q: Are there different forms of pneumonia?
A: Let me give you three examples: 1) Pneumonia developed while in the community which is known as Community Acquired Pneumonia (CAP).
2) Hospital-Acquired Pneumonia (HAP), which is pneumonia acquired during or after hospitalisation for another illness or procedure.
3) Aspiration pneumonia which is the term used to describe a lung infection due to aspiration of contents in the mouth or stomach. This is common in patients who are unconscious, paralysed or patients with swallowing difficulties.
Q: What is the commonest form globally?
A: It varies from time to time. A wide range of different viruses and bacteria is known to cause pneumonia in the community. Streptococcus Pneumonia Bacterium is the most common cause of community-acquired bacterial pneumonia worldwide. Tuberculosis can also easily spread within close communities such as elders’ homes.
Q: How vulnerable are patients with Covid-19 if they get pneumonia?
A: Pneumonia due to Covid-19 was the commonest cause of pneumonia few weeks ago. Covid-19 is a highly contagious infection. Many viruses including Covid-19 cause a simple upper respiratory tract infection, but a less percentage progresses to develop pneumonia. Covid-19 virus itself can cause pneumonia and serious outcome in some patients although Covid-19 causes a mild upper airway infection in more than 80 percent of patients. Some patients develop secondary bacterial pneumonia and even pneumonia due to fungi. In addition to the Covid virus, medicine used in the management of Covid pneumonia may be a contributory factor.
Q: Is it contagious? If so who are those most vulnerable to it?
A: Some viruses such as Covid-19, influenza are highly contagious. Those with lowered immunity are more prone to develop pneumonia. They may develop pneumonia even with less infectious germs such as fungi which normally do not cause pneumonia in healthy people.
Q: Symptoms to look out for?
A: Patients with pneumonia commonly have cough with or without phlegm, fever, difficulty in breathing and chest pain. Some may have blood in the sputum. Sweating, loss of appetite, diarrhoea and confusion may occur.
Q: Are chronic smokers also at risk?
A: Smokers have a high risk of getting pneumonia and its complications.
Q: What about those with asthma and bronchitis?
A: Asthmatics and patients with bronchitis can have more severe symptoms and complications due to pneumonia. Asthma is an inflammatory disease of the airways to the lungs. Triggers which induce inflammation in asthma could be viral infections (colds), dust, smoke, fumes, changes in the weather, grass and tree pollen, animal fur and feathers, strong soaps, and perfume. In acute bronchitis, there is inflammation of breathing tubes due to viruses and less commonly due to bacteria. In chronic bronchitis, there is inflammation of breathing tubes due to smoking and exposure to irritant gases.
Q: How vulnerable are the children? How can they be protected?
A: All age groups ranging from newborn to elderly are affected by pneumonia. The national immunisation program protects infants from some of the bugs causing pneumonia. It is known that pneumonia can be prevented by breast feeding during the first six months of life.
Q: What happens to babies with underlying preconditions such as heart disease if exposed to pneumonia?
A: These babies have a high risk of recurrent pneumonia and may have serious outcomes.
Q: What are the health implications of getting pneumonia? Are they long lasting?
A: Patients with milder symptoms may recover without any complications. Those who have severe disease (caused by more virulent germs, affecting most of the lung tissues, and those who have impaired immunity) may develop serious complications and can even die of pneumonia.
Q: What are the most serious complications?
A: Failure to maintain requisite oxygen level in the body, spread of the infection into chest cavity (Empyema), spread of the infection in to blood stream (Septicaemia), leaking of air into the chest cavity (Pneumothorax), coughing up blood, are some of the serious complications of pneumonia. Those who recover following severe pneumonia can be left with scarring and damaged lungs. These patients may continue to have breathing difficulties and recurrent chest infections.
Q: How is pneumonia transmitted?
A: Bugs having the capacity to cause pneumonia enter into the lungs during normal breathing. These bugs could be from the infected materials from a patient with pneumonia. The surfaces could be contaminated with particles containing bugs which get the access to our lungs when we touch our face with contaminated hands. Bacteria can spread into lungs in unconscious or patient with neurological illness.
Q: How is pneumonia diagnosed?
A: Pneumonia can be diagnosed or suspected after talking to the patient and doing a physical examination. Physical examinations and bed side assessments will help in assessing the severity. The diagnosis can be confirmed by doing a Chest X-ray. Various blood tests, urine analysis, sputum and nasal/throat swab for PCR testing will be necessary to detect the severity of the illness, complications, coexisting illnesses such as diabetes, liver, heart and kidney diseases, and also to identify the exact causative agent (type of virus, bacteria, fungus).
Q: If a patient comes to you with symptoms of pneumonia, what is the first thing you would do as a Pulmonologist?
A: I would quickly assess the vital parameters (pulse, blood pressure, respiratory rate and the body temperature) and the oxygen saturation and decide whether immediate attention is needed. If the patient is ill, type of antibiotics, antiviral treatment in addition to fluid management and oxygenation will be decided and will be started immediately.
Testing will be carried out at the same time. The patient will be closely monitored. Giving assisted breathing support and HDU, ICU care will be arranged accordingly.
Q: Does the patient require hospitalisation?
A: Hospitalisation will be decided depending on the severity of the illness and also considering their social background. Commonly, hospitalised patients are treated with antibiotic injections on admission and later changed over to oral medications. Those who get better without complications would be sent home in a few days and reassessed at the clinic later. Some may need prolonged hospitalisation and even ICU care.
Q: Is there a pneumonia vaccine?
A: There are vaccines to prevent pneumonia due to certain bacteria and viruses. Pneumococcal vaccine, influenza vaccine, Hib, and vaccines to protect from Covid-19 are some of them.
Q: Is here an age group of people for whom these vaccines play a vital role in saving their lives during a pneumonia epidemic?
A: Elderly people are vulnerable to develop pneumonia and its complications. The death rate is also higher in elderly population in whom other illnesses such as diabetes, hypertension, and heart diseases are common. Vaccination plays a vital role in the elderly population.
Q: Can the patient be treated at home, especially if it is a mild form? If so, what home remedies do you suggest?
A: Patients with a mild form of illness could be managed at home. They should rest at home. Temperature should be checked a few times a day or when feeling febrile. Adequate intake of fluid is important. They should get admitted if feeling unwell, breathlessness, having persistent fever or develop new symptoms.
Q: To avoid spreading it to others, what are the do’s and don’ts to follow by those in close contact with the patient?
A: Not all the pneumonias are highly contagious. Your doctor can tell you what type of pneumonia your contact person has and what precautions to be taken to avoid further spread. Covid-19 is highly contagious. Maintaining two metre distance, wearing protective masks by patient and the contacts, washing hands and wearing protective gloves are important for it.
Q: Your message to our readers on how to avoid getting pneumonia?
A: We have a national system of immunisation which protects people against some dangerous bugs causing pneumonia. It is our duty to make sure that children are vaccinated according to the schedule.
Respiratory hygienic measures such as clean hands (through washings or using disinfectants), avoiding coughing or sneezing in front of others without a protective covering, and wearing a mask during an epidemic or pandemic situation, good nutrition and adequate fluid intake are utmost important to keep the immune system active. Peaceful mind and healthy physical exercise will boost our immune system. Controlling other illnesses such as diabetes and avoiding smoking can boost immunity against pneumonia.
