Formerly known as Multiple Personality Disorder, Dissociative Identity Disorder (DID) is a widely misunderstood mental disorder which affects between 0.01 and 1 percent of the population. You have all seen a movie where the killer is found to be some mild-mannered person with a hidden criminally insane personality.
 Dr. Romesh Jayasinghe |
DID has also been mistaken for possession by demonic and other-worldly entities for centuries. Although films tend to stereotype mental disorders to sell a story and religions have mistaken them as spiritual experiences, people with dissociative disorders such as DIDs are real victims and can lead normal and healthy lives despite their challenges; much different to the ones portrayed in cinema.
Although modern psychology have grown in leaps and bounds through years of research, taboos die hard and this stops people from coming out and getting help for their mental health problems. On the other hand, there is also the problem of mental disorders going “mainstream” to the point where they become trends or used by those with malicious intent to get away with their bad behaviour and crimes; as seen with increasing number of people faking depression and other disorders to abuse pharmaceutical drugs. Given the two extremes of either sweeping mental health issues under the rug or trivialising them, the best society can do is to have proper awareness on how to treat and support those living with these challenges.
We spoke to a psychologist and founder of the Institute of Mental Health Dr. Romesh Jayasinghe for some answers to pressing questions regarding DID.
Excerpts
Q: What is Dissociative Identity Disorder?
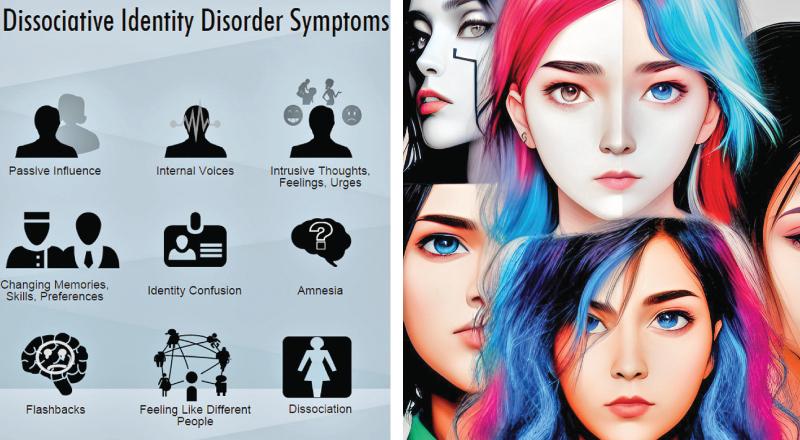
A: In Dissociative Identity Disorder, two or more identities alternate being in control within the same person. These identities may have speech, temperamental, and behavioural patterns that are different from those normally associated with the person. Also, the person cannot recall information that would ordinarily be readily remembered, such as everyday events, important personal information, and/or traumatic or stressful events.
Q: What causes DID?
A: DID is mainly caused by a person being horribly, often unspeakably, abused as a child. This abuse can be physical, sexual or emotional or a combination of these. Most surveys report a high rate of childhood trauma in cases of DID. We now know that DID is rooted in the natural tendency to “escape” or “dissociate” psychologically or emotionally from the unbearable negative effect associated with severe abuse (trauma) or chronic stress. A lack of social support during and after the abuse also is a critical contributory factor.
As children develop, they must learn to integrate complicated and different types of information and experiences into a cohesive, complex personal identity. Sexual and physical abuse that occurs in childhood when personal identity is developing may have lasting effects on the person’s ability to form a single, unified identity, especially when the abusers are parents or caregivers. Children who are abused may go through phases in which different perceptions, memories, and emotions of their life experiences are kept segregated. This segregation of experiences is intensified by parents or other caretakers who behave inconsistently over time (for example, being by turns affectionate or abusive), a behaviour that is called betrayal trauma. Over time, such children may develop an increasing ability to escape the abuse by “going away,” by detaching themselves from their harsh physical environment, or by retreating into their own mind. Each phase or traumatic experience may be used to produce a different identity.
However, if such vulnerable children are sufficiently protected and soothed by truly caring adults, dissociative identity disorder is less likely to develop.
A surprisingly major portion of the cause of dissociative experience could also be attributed to a chaotic, unsupportive family environment. We also note that individual experience and personality factors also contributed to dissociative experiences leading to the possible development of DID. There can also be a biological vulnerability to DID, but it is difficult to pinpoint. There is some evidence of smaller hippocampal and amygdala volume in patients with DID compared with “normals”. Head injury and resulting brain damage may induce amnesia or other type of dissociative experiences.
Q: Can DID be brought under control by oneself?
A: DID is a highly dysfunctional, long term disabling and pervasive mental illness. Usually it is not possible for this disorder to be brought under control by oneself once the disorder has developed and manifested in a person fully, due to the complexity and lack of awareness and understanding of this disorder by the person suffering from this complicated psychological condition. Only with professional psychiatric treatment and psychological trauma based therapy can a person achieve remission of symptoms and in many cases achieve a stable recovery over several years of treatment.
Q: How much can psychotherapy help?
A: Extensive psychotherapy may help people integrate their identities or at least help the identities cooperate. The goal of treatment for dissociative identity disorder is usually to integrate the personalities into a single personality. However, integration is not always possible. In these situations, the goal is to achieve a harmonious interaction among the personalities that allows more normal functioning.
Medications can relieve some specific coexisting symptoms, such as anxiety or depression, but does not affect the disorder itself.
Psychotherapy is the main treatment used to integrate the different identities. Psychotherapy is often long, arduous, and emotionally painful. People may experience many emotional crises from the actions of the identities and from the despair that may occur when traumatic memories are recalled during therapy. Several periods of psychiatric hospitalisation may be necessary to help people through difficult times and to come to grips with particularly painful memories. During hospitalisation, people are continuously given support and monitored.
Sometimes, psychotherapists use techniques such as hypnosis to help such people calm themselves, alter their perspective on the events, and gradually desensitise the effects of traumatic memories, which are sometimes tolerated only in small amounts. Hypnosis can sometimes help people learn to access their identities, to facilitate communication between them, and to control the shifts between them.
Dissociative patients who are not appropriately treated or who attempt to treat themselves tend to get worse and DID then become one of the most difficult to treat psychiatric conditions. Alternate personalities (alters) do not integrate spontaneously. Untreated DID tends to leave the sufferer open to further abuse. The classic treatment approach as described by the International Society for the Study of Trauma and Dissociation (ISSTD) Treatment Guidelines, is called phase-oriented trauma therapy and consists of three phases: 1) stabilisation, 2) trauma-work and 3) integration.
However, no medication exists to address DID specifically. Medications may be prescribed in cases of DID to help deal with the distressing symptoms such as psychosis, anxiety and depression.
Q: Can DID develop into something worse?
A: Unfortunately, if left untreated, DID can develop into more severe forms of psychotic mental illness, such as psychotic depression and even schizophrenia.
People with dissociative identity disorder often describe an array of symptoms that can resemble those of other mental health disorders as well as those of many general medical disorders. For example, they often develop severe headaches or other aches and pains. Different groups of symptoms occur at different times. Some of these symptoms may indicate that another disorder is present, but some may reflect the intrusion of past experiences into the present. For example, sadness may indicate coexisting depression, but it also may indicate that one of the personalities is reliving emotions associated with past misfortunes.
Many people with dissociative identity disorder are depressed and anxious. They are prone to injuring themselves. Substance use disorders, episodes of self-mutilation, and suicidal behaviour (thoughts and attempts) are common, as is sexual dysfunction. Like many people with a history of abuse, they may seek out or stay in dangerous situations and are vulnerable to retraumatisation.
In addition to hearing voices of other identities, people may have other types of hallucinations (of sight, touch, smell, or taste). The hallucinations may occur as part of a flashback. Thus, dissociative identity disorder may be misdiagnosed as a psychotic disorder such as schizophrenia. However, these hallucinatory symptoms differ from the typical hallucinations of psychotic disorders. People with dissociative identity disorder experience these symptoms as coming from an alternate identity, from inside their head. For example, they may feel as if someone else wants to cry using their eyes. People with schizophrenia usually think the source is external, outside of themselves.
Q: Statistically, more women suffer from DID. Why is this?
A: Dissociative identity disorder (DID) is classified by DSM-V as “presence of two or more distinct identities or personality states, each with its own patterns of perceiving, thinking, and relating to the environment and the self” where “at least two of these identities or personality states recurrently take control of the person’s behaviour” (American Psychiatric Association, 2013).
We now know that 1-3 percent of the general population has DID. With a world population of 8.0 billion, that means there are easily 80 million to 240 million.
Females experience more childhood abuse than males at a ratio of 10:1 and thus more females suffer from DID. However, more males who have been abused may experience pathological dissociation. Dissociative identity disorder is typically caused by trauma occurring at less than nine years of age. Early age of abuse onset predicts a greater degree of dissociation. The average number of alternate personalities a person with DID has is between eight and 13, but there have been rare cases reported of more than 100 personalities within one individual.
Q: How did movies, religions trivialise DID?
A: Movies, novels, stories and religions created many misconceptions and myths regarding this disorder in the past and this continues even today. In the past, most religious traditions and beliefs were that a person suffering from this so-called “switching” from one identity or personality to another kind of disorder was in fact possessed by demons or evil spirits or was a victim of black magic. They also created another misconception that such a psychological or psychiatric disorder never actually existed in reality but was only a fictitious disorder or a “pseudo-disease”.
DID has been recognised as a mental disorder since its inclusion in the 1980 release of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III).
The diagnosis of DID continues to remain controversial among mental health professionals as understanding of the illness develops, but there is no question that the symptoms are real and people do experience them.
Q: What can the community do to help?
A: A support network of family, close friends and treatment providers is crucial; people to talk to, have an understanding therapeutic relationship with and build trust with.
Having community support when living with dissociative identity disorder (DID) is an important part of dealing with the disorder. Dissociative identity disorder can feel like a burden in more ways than one. In addition to dealing with the multiple conversations happening in your mind, you need to maintain your “outer shell,” or the parts that other people interact with the most.
Having a condition like DID can often feel like you’re hiding a secret, as is typically the case with many mental illnesses. Because there are no immediate physical ailments that other people can register or notice, the condition mostly goes overlooked.
While it’s easy enough to continue on with your life without coming out about your DID, your life becomes much richer once you do. It can be intimidating to share your secret at first, but there are many benefits to helping the people around you understand the condition you live with every day.
While there is no rule that says you need to discuss your life with DID, doing so can help you build the community support you need. More importantly, you’ll discover that some of the most supportive people you can find are not just family members, but your neighbour, work colleague or supervisor, fellow community member, or your family doctor or physician, your community psychiatrist and other mental health professionals such as your local counsellor or psychologist.
