 |
|
Dr Joel Arduchelvam Elderly persons with diabetes, hypertension, cholesterol most at risk
|
Heart diseases are on the rise globally and in Sri Lanka. The latest World Health Organisation Report 2014 has been quoted as saying that coronary heart disease had reached 32,582 or 25.74% of total deaths in Sri Lanka at the time of its publication.
In 2013, it was reported that twenty persons a day die of heart disease, while according to recent studies those at highest risk of heart disease are from South Asian countries, including Sri Lanka.
According to most cardiologists most heart diseases are preventable with healthy lifestyles, starting from a very early age. However, in advanced cases, they may require surgical intervention. Vascular Transplant Surgery is one of them. To learn more about this surgical procedure, the Sunday Observer spoke to Consultant Vascular and Transplant Surgeon Dr Joel Arduchelvam of the Anuradhapura Teaching Hospital. The latter recently blazed a new trail in vascular and transplant surgery when he headed a team which performed the first simultaneous kidney and pancreas transplantation.
Excerpts…
Q. As a Consultant Vascular and Transplant surgeon how would you describe your field of specialty to our lay readers?
A. Vascular and Transplant surgery involves two fields of surgery. Vascular surgery involves procedures (surgery and endovascular) done on arteries and veins. We deal with all the blood vessels in the body other than the heart vessels (coronary vessels).
Transplant surgery means, taking organs from a donor and implanting it into a patient (recipient) with organ dysfunction (organ failure)
Q. What does it involve?
A. The main areas of workload in vascular surgery in Sri Lanka are for blocked arteries (occlusive arterial disease- OAD), aneurysms (dilated arteries) and surgery for blood vessel injuries. Also, surgery for varicose veins involves a major part of vascular surgical workload.
Q. In Sri Lanka, what is the main organ that is usually transplanted?*
A. The main organ being transplanted in Sri Lanka is the kidney. In addition, liveries are also transplanted occasionally. Recently, the first simultaneous kidney and pancreas transplantation was performed by me.
Q. What is Occlusive Arterial Disease (OAD)?
A. OAD results from blockage of arteries resulting in lack of blood supply. The commonest reason for occlusion of blood vessels is atherosclerosis, which arises as a result of deposition of cholesterol and other substances on the arterial wall. Risk factors for the development of atherosclerosis other than having high cholesterol include high blood pressure, high blood sugar, smoking and lack of exercise.
Q. What symptoms do patients with occlusive arterial disease (OAD) present?
A. Most patients with OAD do not have any symptoms (Asymptomatic). Others present with leg pain (Claudication – Pain while walking or pain on toes and foot at rest), ulcers, or gangrene (death of tissues).
Q. What are the treatments available for OAD?
 |
A. Most of the patients with occlusive arterial disease (those without any symptoms and toes with claudication) do NOT need any intervention (surgery or angioplasty / stenting.)
They only need medications to control their risk factors (high blood sugar, high blood pressure, high cholesterol, etc.) and walking exercise. They should also prevent injuries causing wounds on their feet which will be difficult to heal due to their condition..
Q. So when do they need surgical interventions. What are they?
A. Interventions available for OAD are either surgery or angioplasty. These are offered to patients with OAD and a complication like ulcer or gangrene.
Who will undergo surgery or angioplasty is determined by the severity of the disease, fitness of the patient and the availability of the intervention.
Q. What is the main surgical intervention done for OAD in Sri Lanka? How is it done?
A. Main surgery done for OAD is a bypass ( see figure 1), where an arterial blockage is bypassed using a tube graft. This tube graft is often the patient’s own vein (which is preferred) Synthetic tubes are used rarely.
Q. You also referred to angioplasty. What is the procedure used for this?
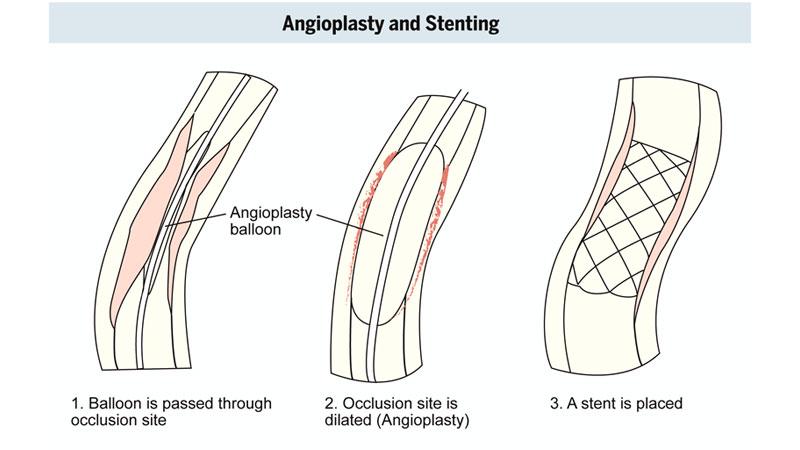
A. In angioplasty, the occlusion is dilated using a balloon (balloon angioplasty and sometimes a metal stent is placed at the site of occlusion
Q. Can any heart patient be eligible to undergo this procedure?
A. No . Patients undergoing a bypass surgery should be fit enough to stand the procedure.
Therefore, patients who are not fit for a bypass surgery are offered an endovascular procedure (angioplasty or stenting).
But the problem with endovascular procedures is that it is not freely available and needs different skills to that of surgery, and the equipment and the stents are expensive.
Q. Once a bypass has been done, how do you ensure it is working well?
A. When the bypass is working well there will be signs of improved circulation to the foot and toes, i.e. feeling a pulse beyond bypass site, reduced or absent pain, improved walking distance, healing ulcers, etc.
 However, the patient is followed up at the clinic to monitor the graft function.
However, the patient is followed up at the clinic to monitor the graft function.
Q. Do most of your patients come to you straightaway or else opt for other treatments?
A. In Sri Lanka, most of the time diagnosis of arterial occlusion as a cause for symptoms and ulcers is delayed. This results in loss of valuable time in saving a limb resulting in amputation.
Q. What advice do you give patients by way of post-operative care?
A. The same disease causing the atherosclerosis can block the bypass graft and the stents. Also, patients with blockage of leg arteries are likely to have blockage of other arteries like, heart (coronary) and brain vessels.
Therefore, even after a vascular procedure patients need to have their risk factors under control (high blood pressure, blood sugar, cholesterol, etc.), by taking their medications regularly and attending clinics regularly.
Also, patients should quit smoking for life. In addition, regular exercise and good dietary routine is essential. They also need to prevent getting foot ulcers in the future.
