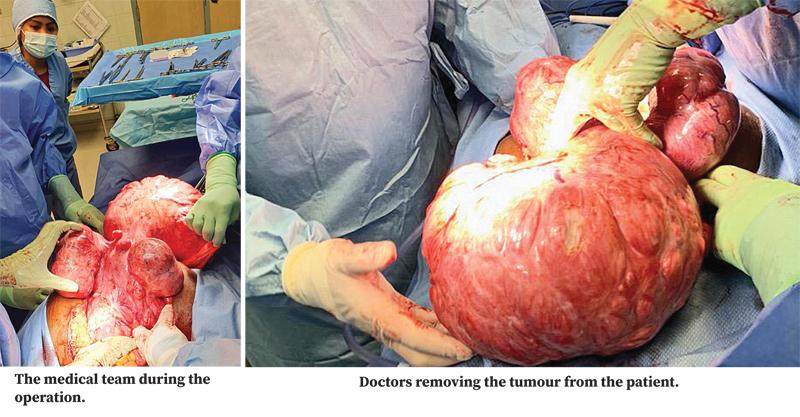
In the Cayman Islands, a team of doctors led by Sri Lankan Dr Sarath Seneviratne, Associate Professor and Senior Consultant, at CTMH, Doctors Hospital, recently removed a giant tumour from the uterus of a patient, which was one of the largest tumours the doctors had ever removed, weighing in at 21 pounds two ounces.
This was likely the largest tumour ever seen by surgeons in the Cayman Islands and one of the largest ever seen in the world with a successful outcome. The team of medical professionals who removed the tumour also includes surgeons Dr Steve Tomlinson and Dr Chris Bromley. “The patient had an abdominal mass extending to the chest and under the liver. She had considerable pain and discomfort, having undergone a surgery previously in London. She needed the mass to be removed,” Dr Seneviratne said.
Experienced team
 Dr Sarath Seneviratne |
It was anticipated that the surgery would take three hours, would present challenges, given the size of the mass. Dr Seneviratne enlisted the assistance of Dr Tomlinson and Dr Bromley, along with a team of nurses who were well-versed in working together as a surgical team. The approach was to ensure every measure was taken to keep the patient safe, the doctor said.
“We anticipated that it would be a difficult surgery and that it would bleed considerably,” Dr Seneviratne said. “The anesthetist, Dr Stephen Gay, put in an arterial line rather than the usual venous line to help control the bleeding, as many patients have died under similar circumstances, through uncontrollable blood loss, renal failure and sometimes other complications, such as a coagulopathy or multiple organ failure.
The mass was under the diaphragm and pressing against the liver, aorta, ureters and kidneys. It had gone into the pelvis. The abdominal wall was so enlarged vertically as well as transversely, that it looked as if there were triplets. The patient had hypertension and weighed over 300 pounds, which added to the risks for anesthesia and surgery.
The size of the patient, the size of the mass and the intra-abdominal adhesions were the largest difficulties, because it had attached itself to various parts of the patient’s internal organs, including the small bowel, rectum, bladder and pelvic wall, hence increasing the risk of bleeding.
During the surgery, she was bleeding profusely from all sides of the tumour, especially from behind the mass. Hemostatic clamps and large warm packs were used to control the haemorrhage, while meticulously ligating the vessels.
Basic principles
“We had to stick to basic principles of surgery,” Dr Seneviratne said. “The basic principles are: a) you have to stop the bleeding and b) approach it in such a way that she won’t bleed,” he said.
The doctors had to move quickly to remove the mass, trying to remove it in one piece so it could be examined histologically as a whole, to look for malignancies. The doctors kept the tumour in a large bucket before it was flown to the US to be examined. They managed to save one ovary and the patient went home three days later in good health,” Dr Seneviratne said.
Assisting surgeon Dr Christopher Bromley said that he had looked at the size of the patient’s stomach with some concern before they began to operate.
“I could also see it was going to be a substantial operation,” he said.
Dr Bromley said that the operation began smoothly and continued so with Dr Seneviratne performing the surgery “extremely expertly”. However, when they uncovered the tumour he said he was “truly over- awed” at its size. “It went way beyond my experience, probably the largest I had seen,” he said.
“It was the largest uterine fibroid that I had seen,” assisting surgeon Dr. Steve Tomlinson said.
“The surgery went like clockwork and did not take that long considering the amount of work that had to be done, especially when you consider that a normal hysterectomy takes about an hour. We had a great team – it’s really nice when a team is used to working together and can anticipate whatever the surgeon needs. Everything went well.”
Dr Seneviratne said, “You need an experienced team who are on the ball because we needed 27 needles and sutures, which needed to be constantly given to the surgeon. It’s a synchronised exercise where everybody knows what they are doing. It was a great experience for the team.”
