As COVID 19 cases continue to surge, many people caught up in the swirl of fear and panic that has spread due to myths and false rumours on social media are still trying to figure out the actual cause of the virus and what the health authorities are doing to protect them. Media Coordinator from the College of Community Physicians of Sri Lanka (CCPSL) Dr Kapila Jayaratne discusses the facts of this new evolving disease that still baffles medical experts, the early symptoms, tests available for those with suspicious symptoms, and most importantly how to protect oneself effectively .
 Excerpts of the interview with the Sunday Observer…
Excerpts of the interview with the Sunday Observer…
Q. COVID-19 has led to fears and myths about the disease. Many still don’t understand what this new disease is. Please explain what exactly COVID 19 is and how it occurs?
A. Covid19 is a mild to severe respiratory illness like a common cold, caused by a virus called Covid19. The virus is found to spread mainly from person to person, mostly through respiratory droplets produced when an infected person with the illness coughs or sneezes. These droplets can deposit in the mouths or noses of people nearby or can be inhaled into the lungs. It can also spread if a person touches a surface with the virus on it and then touches his or her mouth, nose or eyes. This virus can transmit among people when they are in close contact with one another (within about 1 metre).
Q. I understand the virus comes in waves and clusters. At what stage are we? Are we heading towards Italy or Spain?
A. The problem with Covid19 is high infectivity. An infected person can transmit the disease within 5 days to 2 -3 people and 406 people in 30 days. As such the number of cases can exponentially increase within a limited time. This is called an epidemic. Epidemics follow continuously increasing cases, reach a peak and eventually resolve, whether responding to interventions or having exhausted the supply of susceptible persons. Such an outbreak progresses through the following stages;
Stage 1:
No cases - No reported cases
Stage 2:
Sporadic cases - One or more cases, imported or locally acquired
Stage 3:
Clusters of cases - Most cases of limited transmission linked to chains of transmission of either being exposed to a family member being exposed (family cluster) or to neighbours or other close contacts (village clusters)
Stage 4:
Community transmission -Cases without an epidemiologic link are common in the community
Apparently we are in stage 3 either with family or village clustering of cases.
I don’t think we are heading towards what we see in Italy or Spain since we have taken many of the measures well before the epidemic began.
Q. Suspicious symptoms to lookout for?
A. The most common symptoms of COVID-19 are fever, dry cough and shortness of breath or difficulty breathing. Other symptoms can include: tiredness, aches, runny nose and sore throat. Some people have experienced the loss of smell or taste. The severity of COVID-19 symptoms can range from very mild to severe. Some people may have no symptoms at all. If you have the above symptoms or you've been in contact with someone diagnosed with COVID-19, go right away for medical advice.
Q. What are the tests used to detect them?
A. We can suspect the disease with symptoms and signs. Laboratory testing can be performed to detect the presence of virus and those that detect antibodies produced in response to infection. To test for COVID-19, a long swab will be used to take a nasal sample. The sample is then sent to a lab for testing. The RT-PCR test is done to detect the presence of viruses in samples. This test is specific and is designed to only detect the RNA of Covid19 virus. It is used to confirm very recent or active infections. The RT-PCR test performed with nasal or throat swabs is only reliable in the first week of the disease. Later on the virus can disappear from the throat to localize and multiply in the lungs.
In patients who have recovered from Covid-19 or may have carried the virus without realizing it, a serological test can show who carries antibodies, even if the virus is no longer present. Antibodies are proteins that help the immune system identify and eliminate threats. Once they’re made, they help the body neutralize future infections from the same threat.
Q. The quarantine period in Sri Lanka is two weeks. Is this the same as in other countries?
A. Quarantine is usually practised for the incubation period, two weeks, of the disease. Usually, this is the same for many countries.
Q. If a person tests positive for COVID-19 can he/she get it again?
A. The emerging consensus is that becoming re -infected after recovering is highly unlikely.
Q. The World Health Organization (WHO) declared Covid19 as a 'public health emergency' .As the College of Community Physicians of Sri Lanka (CCPSL) is the apex professional body for the practice of public health in Sri Lanka, how did you respond to this challenge?
A. Countries can change the course of the pandemic, if the basic public health principles are adopted as guided by the WHO based on country-specific contexts. In this respect, the CCPSL strongly advocates that the current COVID-19 epidemic in Sri Lanka be controlled through a strong-willed, evidence-based public health response. In response, under the directives of the Minister of Health, Secretary, DGHS and Additional Secretary Public Health, the following preventive health teams have been in operation consistently:
- At national level - Deputy Director General Public Health, Directors in Public Health (Epidemiology Unit, Quarantine, Health Promotion Bureau, Disaster Management, Family Health Bureau), consultant community physicians, medical officers, special grade public health nursing officers and other staff supporting all the public health programs are contributing at their highest capacity.
- At Provincial and District level – The Provincial Director, Regional Director, consultant community physicians, medical officers, special grade public health nursing officers, special grade public health inspectors and all Provincial and District level staff and at Divisional level, led by the regional epidemiologists, medical officers of maternal and child health (MO-MCH), medical officers of health (MOH), public health nursing sisters, public health inspectors, public health midwives and all other categories work as a team which has shown a remarkable sense of teamwork.
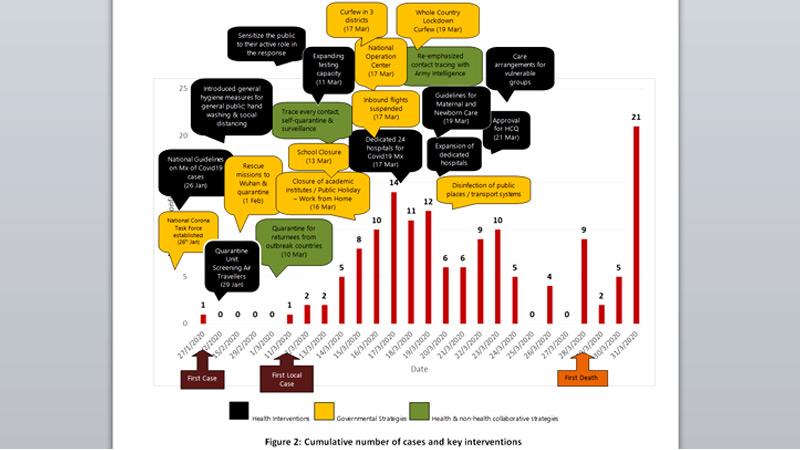
The case load could have been many more if not for the effective interventions initiated by public health teams in traveller screening, case detection, contact tracing, early reporting, early isolation / quarantine and mass health education coupled with other strategies which were in place. The public health efforts resulted in containing the epidemic without progressing to the stage of community transmission.
Q. How can we control the epidemic?
A. We have three options: Totally containing the outbreak at a very early stage, flattening the curve and raising health system capacity. “Containment” through a comprehensive approach (first response) would still be the major objective as the cases originating from local transmission are few. We also consider ‘flattening the curve’ as the next best to slow the coronavirus spread.
Q. What is “flattening the curve”?
A. Keeping the patient load at any given time at a level manageable by the health services. That is to slow down the transmission of the disease so that the health services will not be saturated. Usually, it takes approximately 2 weeks from the appearance of the first few cases to the onset of a larger outbreak. This interim period is the most crucial time for timely and appropriate public health measures.
Q. The focus now being mainly fighting COVID-19 , the danger of Non Communicable Diseases which also claim hundreds of lives in this country could be sidelined. Your comments?
A. I agree. When the whole system is geared to protect people from Covid19, the focus for other disease entities and non-Covid patients will be diluted. At present, it seems the entire health system is geared to face the challenge of Covid19 at the expense of services at First Contact level, Clinic-based care, field health services, surgical care and other routine interventions. We believe the disruption of the whole spectrum of routine services in the entire country is unnecessary.
The consequences of this would end in a long term catastrophe. Therefore, it is essential to introduce triage systems, reserving tertiary main hospitals for non-COVID patients.
As a country with a relatively low COVID-19 caseload, it is essential to maintain routine service delivery. Maintaining supply chains for medications and other needed supplies should be done by a high-powered team as importation may be compromised due to high demand and limited supplies from manufacturing countries.
Q. How are pregnant women who are especially vulnerable at this time protected?
A. They have been educated on protective measures and asked to stay home, avoid crowded places, not go shopping and contact public health midwife in any emergency. Guidelines to continue clinic care for all high risk and more than 32 week gestation pregnant women both at field and hospital levels have also been sent. They can come to the hospital at any time if they encounter any health problem.
Q. Stigma against COVID patients or suspected patients is one reason why those with symptoms don’t come forward to be tested. What is the CCPSL doing to educate the public that COVD is just another disease?
A. The stigmatization continues to be a major hindrance for case detection and contact tracing. Stigma can drive people to hide the illness to avoid discrimination, stop people from seeking health care immediately and prevent people from adopting healthy behaviors. We have started a massive media and social media drive to address disease stigma. The efforts should originate from healthcare staff up to the general public. Revelation of certain personal identifiers by different health officials to the media should be stopped.
Q. Your message to the public on how to detect early, who to contact if one has suspicious signs, and most importantly prevent contracting COVID-19?
A. Prevention is the best option. Stay at home. Do not go out unless it is essential. If you happen to go out practise social distancing. Frequent hand washing with soap and water plays a key role and also important is your respiratory etiquette. If you or one of your family members experience fever, cough, cold, shortness of breath or sore throat, contact heathcare providers. Tell them your possible contact and travel history. Oblige with health advice. With these, you are safeguarding your health,, your family members’ and the entire community’s health.
