NHSL Stroke Unit offers complete package of treatment, care for stroke patients
 Stroke is one of the most debilitating non communicable diseases one can have. It is the third leading cause of death in Sri Lanka, and of disability. Disturbingly, younger adults are now getting strokes which health officials say are mostly due to changes in lifestyles, stressful work environments and abusing alcohol and smoking. While some factors that trigger stroke are non modifiable, such as age or genes, others such as, unhealthy lifestyles if modified can certainly minimize risks of stroke .
Stroke is one of the most debilitating non communicable diseases one can have. It is the third leading cause of death in Sri Lanka, and of disability. Disturbingly, younger adults are now getting strokes which health officials say are mostly due to changes in lifestyles, stressful work environments and abusing alcohol and smoking. While some factors that trigger stroke are non modifiable, such as age or genes, others such as, unhealthy lifestyles if modified can certainly minimize risks of stroke .
The Sunday Observer spoke to Secretary, National Stroke Association of Sri Lanka, and Consultant Neurologist, National Hospital, Sri Lanka, Dr Gamini Pathirana for more insights into the subject.
Excerpts...
 Q. Many people tend to mistake stroke for other diseases with similar symptoms. As a neurologist, how would you describe stroke?
Q. Many people tend to mistake stroke for other diseases with similar symptoms. As a neurologist, how would you describe stroke?
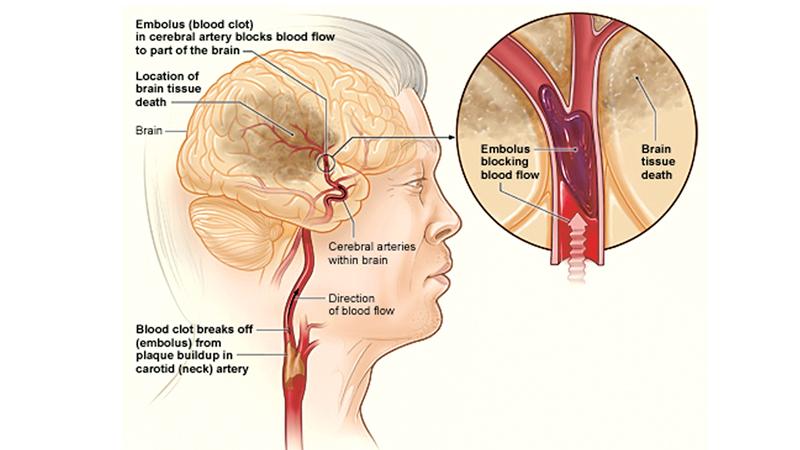
A. Stroke happens all of a sudden. Sudden loss of function is the best way to recognize a stroke. This is due to loss of brain cell function due to acute loss of blood supply. Blood clot blocking an artery (pipe that takes blood towards brain) is one form of stroke.
Q. Are there different types of strokes? Can severity of the stroke vary in each type?
A. There are two kinds of stroke, the first and the more common being ischaemia (blood supply is blocked by a clot in an artery) and second is, haemorrhage ie: rupture of an artery leading to blood leaking into brain matter. In both situations, death of brain cells take place due to loss of blood supply and the pressure effect. Severity of stroke depends more on the extent of damage within the brain than the type of stroke.
Q. What are the trigger factors that cause a stroke?
A. They are better called ‘risk factors’ because you need to get exposed to those factors for a period of time before stroke occurs. Among them are, uncontrolled high blood pressure, sugar or lipids, lack of exercise, obesity, smoking, alcohol abuse, mental and physical stress. Lack of knowledge about stroke also is a risk factor for future development of stroke. ‘World Stroke Association’ advises people to be knowledgeable about stroke and keep talking to each other to better understand this disease
Q. Symptoms?
A. Sudden onset of weakness in either the arm or leg (monoplegia), arm and leg on the same side (hemiplegia), sudden loss of speech, balance and vision are some symptoms of stroke. Stroke symptoms are generally obvious but can be subtle that you hardly notice it, and rarely, stroke can be asymptomatic too, discovered on a CT scan done subsequently for some other reason.
Q. A few decades ago, stroke, like other non communicable diseases, was considered an illness primarily associated with old age ( those above 55) Today, there seems to be a disturbing shift in the age pattern with younger people getting stroke. Do you agree?
A. Yes. Age is a non-modifiable risk factor for stroke, meaning as you grow older the chance of having a stroke increases. This chance is brought about by the interplay of many risk factors. It is true that we see more and more young individuals presenting with stroke. This shift may be due to changes in lifestyles, stressful work environments, bad eating habits and abusing alcohol or smoking etc. Stroke can rarely be familial where they present at a younger age.
Q. How does stroke rank in our country at present?
A. In Sri Lanka, stroke lies at third place as far as deaths are concerned. A third of stroke patients die, another third survives with dependency and the other third survives with independency. As far as disability is concerned stroke is the leading cause of adult disability competing with trauma related disability in younger population. Every one in six will suffer a stroke during their lifetime. 80% of stroke burden is with low and middle income countries like ours, while 90% of stroke patients had 10 avoidable risk factors.
Q. Genderwise, is it correct that more older women get strokes than men? If so why? Is it because women live longer than men? Or has it something to do with their depleting estrogon hormones?
A. Women do have a protection from oestrogen hormone until menopause, where incidence among men is higher than women. This becomes equal after menopause. After 75 years of age we see more women presenting with stroke due to higher life expectancy, meaning more women are alive at this age to present with stroke.
Q. Is it correct that among other pre-existing non communicable diseases, high blood pressure or hypertension is the biggest cause for stroke?
A. High blood pressure contributes to most strokes. Of the risk factors, high blood pressure is the main risk. It causes both ischaemic and haemorrhagic types of stroke. High blood pressure has no symptoms. So, taking blood pressure pills when you feel you are having blood pressure is wrong. Control of high blood pressure could bring down stroke incidence significantly. Blood pressure control is helped by low salt in diet, avoid smoking and alcohol abuse, reduce stress, regular exercise and drugs used to reduce blood pressure. Tablets prescribed by your doctor to reduce blood pressure needs to be taken regularly, everyday.
Q. What should be the ideal level of blood pressure in a person already having this condition?
A. If your blood pressure is above 140 /90 with repeated checking you are said to have high blood pressure. Goal for treatment is 140/90. But the exact goal can vary with each individual, so it is set by your treating physician.
Q. What are the other known risk factors? How do they directly or indirectly lead to a stroke?
A. The modifiable ones are Diabetes Mellitus, dyslipidaemia, smoking, physical inactivity. Uncontrolled Diabetics have approximately twice the risk compared with those without Diabetes. Most above factors cause atherosclerosis meaning deposition of lipid rich plaques on the inner side of arteries leading to what is called ‘atherothromboembolic stroke’. Atrial fibrillation is a heart condition leading to clot formation within the heart leading to what is called ‘cardio thromboembolic stroke’. Carotid stenosis (CAS) also is a risk factor for major stroke in those who already had CAS related stroke. CAS is treated by a surgical procedure called ‘endarterectomy’ or placement of a ‘stent’ into the carotid artery (like the stents put into coronary arteries in coronary artery diseases).
Q. When a person shows symptoms of a stroke what are the first key rules to follow prior to admitting the patient to a hospital?
A. If one loses hand or leg strength, mouth deviation, loss of speech, balance or swallowing, all of a sudden you may suspect stroke. If you want further proof ask the patient to smile (or show teeth) to look for mouth deviation, ask patient to lift both hands up looking for weakness of one arm over other. Ask a question, get the patient to speak to find whether speech is lost or intact.
If you think patient had a stroke note down the time and rush patient to the closest hospital.
Q. What is the treatment procedure followed ?
A. Treatment of stroke depend on whether it is ischaemic (blocked artery) or haemorrhagic (ruptured artery) which can be differentiated by a CT scan done in the early hours. If patient presents later than 10 days CT scan may not differentiate this. For ischaemic variety if patient presents very early within 4-6 hours patient will be evaluated for thrombolysis (clot lysis) or thrombectomy (clot removal by a catheter).
Furthermore, doctors would pay attention to swallowing difficulties, hydration, nutrition, sugar control, blood pressure control and temperature control. Stroke is not a disease of an individual but, a disease of the whole family. So, the stroke team goes on to speak with the family, identify problems and give help that they need.
Q. How soon should a person be brought for treatment once he gets a stroke?
A. As early as possible. Doctors request patients to be brought within 4-5 hours because suitability for clot busting treatment is within that period.
Q. If there is a delay what happens?
A. The delay in presentation prevents receiving early acute treatment, and prevents getting ‘early CT’ scan which differentiates the type of stroke. After ischaemic stroke certain cells die immediately and others die slowly. Doctors have time to save those threatened cells which die slowly if patient is brought early. Saving brain cells may mean for example, saving ability to walk independently or saving your ability to swallow without tubes in the long run, etc. Rarely stroke like presentation can occur due to bleeding into the tumour in the brain with a sudden presentation where delayed arrival creates more problems for the patient.
Q. Is treatment usually with drugs?
A. There are non-drug options too. Proper positioning on the bed in the early hours prevents complications. Early swallowing assessment and taking measures to prevent deep clots in immobile leg by applying stockings are some non-drug measures.
Early institution of physiotherapy is important in getting the best long term functional outcomes. Stroke care is a team work. Most of the things happening with therapists, social worker and counsellor are non-drug measures which has a major effect on the outcome.
Q. When is surgery needed?
A. Within hours from stroke some stroke patients need clot retrieval (also called thrombectomy). Few patients with stroke due to haemorrhage need evacuation of the clot.
Others with life threatening strokes with significant pressure effect within the brain may need decompression by removing part of bone overlying affected brain. This is a lifesaving procedure more than reversal of the neurological disability. Most patients with stroke do not need any surgery.
Q. The Stroke Unit at the Colombo Hospital is one of the few if not the only unit that has everything a stroke patient needs for multiple team care under one roof.. Your comments
A. The . NHSL (National Hospital of Sri Lanka) had its stroke unit for many years. It has been provided with the multidisciplinary team to look after patients. To develop a stroke unit you do not need much financial allocation. It is a matter of accumulating available facilities to one geographic area in the hospital. Stroke units are known to have improved outcome going by scientific evidence from world over. National Stroke Association of Sri Lanka (NSASL) which is a charity organization comprising neurologists, other doctors and stroke care supporters has made its representation to the Ministry of Health (MOH) to establish stoke units in many hospitals in the country. The main one is under construction at Mulleriyawa Hospital and several other stroke units are being constructed by the MOH. . But, considering the number of stroke patients admitted to hospitals, and the fact that they need a long stay, only a minority gets the chance of having a stroke unit bed.
Q. As a doctor at the NHSL, who comprises this team of stroke carers? What are their specific roles?.
A. The leader of the team usually is a neurologist or a physician with experience in stroke care. Team should comprise physiotherapists, occupational therapists, speech therapists, stroke nurse, social worker and counsellor. All of them have a goal of improving function of the patient. The Physiotherapist would concentrate on gait and balance, occupational therapist on improving activities of daily living trying to make them independent. Speech and language therapist would try to improve the swallowing difficulties and speech and communication. Social worker’s duty is to look into financial side and other social factors affecting the patient and the family. The Counsellor will relieve the psychological suffering by speaking to them.
Q. How long does it take for a stroke patient to recover?
A. This varies. Some may recover within days, others may take a month or even longer. Some may suffer a residual deficit which is going to remain for life. Once a patient gets a stroke there are a few worries. Am I going to die of this? If the patient is admitted to hospital, the chance of this is minimal. Second question, am I going to have long term disability and can I do anything to prevent such disability? Immediate admission and acute treatment is known to reduce long term disability. Early aspirin or other antiplatelet treatment reduces long-term disability. A good rehabilitation program in a proper stroke unit also will reduce long term disability.
Q. Once he goes home can he lead a normal life?
A. We want them to be independent for ‘activities of daily living’. Patient may improve in certain activities and remain disabled with others. When patient’s improvement is not adequate therapists modify the environment to suit his disability. This is done by certain utensils specific for such disabilities, for example, using wide handled spoons or pens, having railing along the walking path, having bars to hold when sitting and getting up in the toilet, etc.
Q. If he is a married man can he resume normal marital relationships? How soon after the stroke?
A. Marital relationships can be started sooner. Post stroke depression and erectile dysfunction sometimes associated with stroke may affect this, but doctors have answers for them when patient discusses these issues.
Q. Can he go back to work? If he is in a physically tiring job, should he opt for a less strenuous job?
A. We want them to get back to work as fast as possible. We always try to get them back to the original job.
Q. What kind of exercise do you recommend for a stroke patient?
A. There are specific exercises depending on the stroke disability to keep their function and prevent disability getting worse. Regular moderate exercises preferably walking, cycling, swimming are useful. Keep working with your physiotherapist periodically to plan your exercise program. Supervision may be necessary for certain individuals when there is risk for falls.
Q. What are the new hi tech inputs the world has seen with regard to identifying stroke risks ahead of time and preventing them? Are they available here?
A. In countries where medical information is electronically stored it is a possibility to use them in alerting individuals not only on stroke risk but on risk for cardiac and other diseases too. These are costly options but hopefully will be a reality soon. It may not be far when your iPhone alert your stroke risk and tell you what you should be doing to reduce the risk.
Q. What are your present obstacles in dealing with stroke victims?
A. The main problem is inadequate stroke unit beds. Trained staff too is a rarity. We need more therapists dedicated for stroke care.
Q. Finally, your word of advice to patients and, relatives on the golden rules to follow before and after a stroke .
A. Check your blood pressure, sugar and lipids periodically. Exercise regularly, quit smoking and alcohol abuse. Prevent stress at workplace by keeping to quantum of work that you are physically able to do. If you had a mini stroke or TIA (Transient Ischaemic Attack) take it as a warning and meet your doctor, get yourself checked to prevent major life threatening or disabling stroke. If you are a stroke survivor with dependency, take your medications, regular checks, and try and join a ‘stroke support group’ where you can meet people with similar problems, and share yours with others how they are coping with them.
