
Latest data indicate, there were 112 maternal deaths in 2016 reflecting a maternal mortality ratio of 33.8 per 100,000 live births. The infant mortality data available from the Registrar General’s Department (2013) reports a rate of 8.2 per 1,000 live births. When translated into numbers, it comes to 2,715 deaths. Both indices are the best in the region. They are also on par with similar rates of highly developed countries, Health Ministry officials have pointed out.
However, despite this impressive record, they are worried that these deaths, however low the prevalence rate, should occur at all in, especially, pregnant women, given the fact that a majority of these births take place in Specialized hospitals, where an obstetrician and theatre facilities are available – 94% and in Non-specialized hospitals 6%. Only 5% of all births are reported from the Private sector. They are also concerned over the slight, but nonetheless, disturbing spike in maternal deaths in recent years.
The Sunday Observer asked the National Program Manager overseeing Maternal and Child Morbidity and Mortality Surveillance for the Health Ministry, Dr Kapila Jayaratne, the causes for these deaths and how they could be prevented, to ensure safe motherhood for all Lankan mothers.
Pre-existing illnesses, especially heart disease, is the most common cause of death over the last few years
Excerpts…
 Q. I understand, most deliveries by Lankan mothers take place in state hospitals equipped with proper facilities. Yet, despite these free specialised services available to them, a relatively high number of mothers and infants die. As the National Program Manager overseeing Maternal and Child Morbidity and Mortality surveillance for the Health Ministry, how serious is the problem today, as compared to some years back? What are the prevalence rates of 1) maternal mortality 2) infant mortality, according to your latest data?
Q. I understand, most deliveries by Lankan mothers take place in state hospitals equipped with proper facilities. Yet, despite these free specialised services available to them, a relatively high number of mothers and infants die. As the National Program Manager overseeing Maternal and Child Morbidity and Mortality surveillance for the Health Ministry, how serious is the problem today, as compared to some years back? What are the prevalence rates of 1) maternal mortality 2) infant mortality, according to your latest data?
A. As a country, we have achieved impressive gains in maternal care service delivery. For example, in 2016, there were 331,073 live births in the entire country. Latest data indicate there were 112 maternal deaths in the same year with a maternal mortality rate ( MMR) ratio of 33.8 per 100,000 live births.
The infant mortality data available from the Registrar General’s Department (2013) reports a rate of 8.2 per 1,000 live births. When translated into numbers, it comes to 2,715 deaths. Both indices are the best in the region. They are also on par with similar rates of highly developed countries.
Q. Let’s consider mothers first. What stages of her period of pregnancy puts a mother most at risk to health impacts that may lead to death, and why?
A. The average length of gestation is 280 days, or 40 weeks, from the first day of the woman’s last menstrual period. This pregnancy period is divided into three trimesters. Each trimester carries different risks depending on the cause of illness.
However, a majority of near-misses and deaths have occurred around or after the delivery.
Pre-existing illnesses, especially, heart disease, is the most common cause of death over the last few years. Many medical diseases are aggravated in the third trimester. Pneumonia, dengue fever and other respiratory illnesses are other common causes.
Obstetric haemorrhage, infections and pregnancy induced hypertension are the three direct causes. They are directly related to obstetric status and these three complications can happen in the pregnancy period or even after delivery of the baby.
First trimester; Ectopic pregnancy -The pregnancy is implanted outside the cavity of the womb. If it is implanted elsewhere there is a risk of rupture and internal bleeding. If action is not taken in time to replace the loss and control the bleeding death can occur.
Second and third trimester; Pregnancy induced hypertension leading to fits causing aspiration of stomach contents or resulting in rupture of blood vessels in the brain and other important body organ failure can cause death of a pregnant mother.
Heavy vaginal bleeding can happen in any trimesters of pregnancy with separation of placenta leading to massive bleeding.
Infections, especially, septic abortion kills mothers in early pregnancy. Infections also can occur after the delivery of the baby leading to blood infection and maternal death. Following emergencies are rarely possible during and after delivery; rupture of the uterus, Amniotic fluid embolism -the mixing of the fluid in the womb with blood, Postpartum haemorrhage -bleeding from the lax uterus after birth or puerperal sepsis -bacteria infecting the reproductive organs.
Q. How do you detect them?
A. Danger signs during pregnancy are; vaginal bleeding convulsions/fits severe headaches with blurred vision fever and too weak to get out of bed severe abdominal pain fast or difficult breathing Sudden release of water from the vagina Little of no foetal movement Bleeding may be due to many causes; Placental abruption, abnormal placenta, rupture of the uterus etc.
 Vaginal bleeding is usually seen outside or rarely internal bleeding can occur. Mother may complain of feeling faintish, excessive thirst, lifeless, difficulty in breathing.
Vaginal bleeding is usually seen outside or rarely internal bleeding can occur. Mother may complain of feeling faintish, excessive thirst, lifeless, difficulty in breathing.
Signs will be loss or altered conscious level, drowsiness, increased breathing, increased pulse rate, drop of blood pressure.
Infections can be inside the uterus and the pregnancy content or other sites such as chest, urinary tract, wound infection and blood infections. Fever and malaise, general aches and pains, shivering, are the symptoms and signs of infection. Early detection and treatment with antibiotics can control the infection properly, otherwise it can spread to blood and cause more severe disease and death.
Illegal attempts on removing the foetus may end in septic abortion. This is also a significant cause of maternal death. Fever, foul smelling vaginal discharge severe abdominal pain and tenderness will be found in abdominal and vaginal examination.
High blood pressure in pregnancy can cause many complications including death. Severe headache, visual disturbances, vomiting, upper abdominal pain and reduced urine passage with or without legs and body swelling, are the symptoms of pregnancy induced hypertension.
If the blood pressure is above 140 /90 mmHg, pregnant or women who have delivered recently should come to a hospital. In pregnancy, routine screening is done with blood pressure monitoring in the antenatal clinics.
Q. What about mothers with mental problems and those with pre-existing conditions ?
A. Every year, in Sri Lanka, 25 – 30 women commit suicide during pregnancy or one year after termination of the pregnancy. This is a big problem and we have taken many measures to address the issue. In the antenatal period past and present mental problems are assessed routinely by field healthcare teams. A majority of mental problems occur during postpartum period (after delivery)
Q. Could a delay in getting to hospital be a contributory factor in the rising spike of maternal mortality?
A. In the Sri Lankan health system, each pregnancy in the country is registered, documented and followed up at household level by the public health midwife.
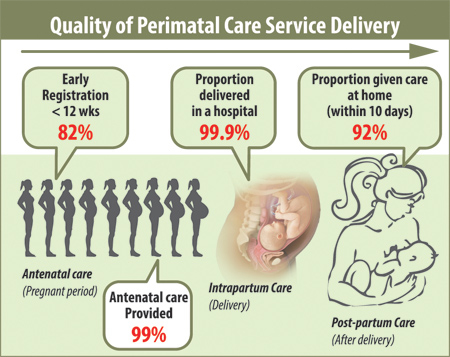
The registration of all pregnancies before three months is 82%, provision of care during pregnancy, either at the field or hospital level, is 99% and proportion delivering at a hospital is 99.9%.
A majority of these births take place in Specialized hospitals, where an obstetrician and theatre facilities are available – 94% and in Non-specialized hospital 6%. Only 5% of all births are reported from the Private sector.
Q. What are the gaps you see in managing pregnant women and infants within your system?
A. There are no issues in managing a pregnant woman or an infant within the existing government hospital network. There may be situations where specialized inputs and or facilities are needed in caring. We have an effective referral system.
If a pregnant mother comes to a peripheral hospital, they can be referred to next level within a short time period. An effective ambulance network is in operation.
However, there are several near misses and deaths among pregnant mothers and children due to the lack of senior support, inadequate facilities or without transfer options.
The Perinatal Society of Sri Lanka initiated the establishment of a support group of senior experts from three specialities (paediatrics, obstetrics, community medicine) to help peripheral level clinicians or junior colleagues to provide expert advice or to take over the case when they are in desperate situations with a critically ill patient -SCOPE (Syndicate of Community Physicians, Obstetricians and Paediatricians in Emergencies).
Mobitel provides the dedicated hotline 3636 for emergency help for junior consultants and peripheral hospital doctors who are managing obstetric, neonatology or public health emergency patient or situation.
Q. Are there national guidelines on pathological post-mortems to find out why they die? I understand that though they exist, they have not been clearly spelt out and the PSSL has stepped in to fill this gap. Your comments?
A. Cause of death (COD) is an essential element of feto-infant mortality statistics. This is crucial in the prevention of feto-infant deaths. COD determination in both, Registrar General’s Department (RGD) and Indoor Morbidity & Mortality Register (IMMR) is not complete or accurate.
Analysis of hospital mortality data indicates that for a major proportion of infant deaths a valid COD is not given. Perinatal data received from hospital to Family Health Bureau also lacks objective COD.
One way to overcome the issue is conducting pathological post-mortems (PPM) for cases for which a valid COD could not be given.
Q. What about foetal abnormalities? How do you detect them? Do you have sufficient facilities for this? Where?
A. Congenital abnormalities are caused by problems during the foetus’s development before birth. Every year nearly 6,000 children are born with an abnormality. In majority (>90%) of the pregnancies, a detailed ultra sound scan is done routinely around 18 – 20 weeks. Many of the structural abnormalities of the foetus is captured by this.
There are other blood tests done in suspected or high risk mothers that can detect certain abnormalities.
Medical Research Institute ( MRI) in Sri Lanka does some investigations related to birth defects. The Human Genetics Unit of the Faculty of Medicine, University of Colombo is one of the major centres providing genetic testing in the country.
Q. Some of these deaths occur when the mother returns home. Within how many days of returning home do most mothers and babies suffer from health setbacks that put their lives on the line?
A. If we consider quality care, 92% of women after delivery have been cared for by our public health midwives at their doorstep, within 10 days.
There may be post-partum morbidities (illnesses) like fever, shortness of breath, sepsis, bleeding, high blood pressure, mental health issues and aggravated existing diseases, especially, heart diseases. Women need to come back immediately to the hospital if they experience such danger features.
Q. I understand, the Perinatal Society of Sri Lanka ( PSSL) has introduced certain quality dimensions for safe motherhood. What are they?
A. Providing a female companion during labour is one. Obstetric units in Sri Lanka that are allowing female labour companions have reported positive results of this intervention within existing facilities.
The presence of a companion during labour is said to be one of the most effective interventions in labour. It has been proved to have benefits on the process of labour, for the mother and the neonate.
These include lesser requirement of pain relief, shorter labour, higher chance of a normal delivery, higher maternal satisfaction and better establishment of breastfeeding.
Pain relief in labour is also an option on request to mitigate suffering during labour.
Q. Finally , your word of advice to new mothers and their care givers .
A. As I said, infections, especially septic abortion kills mothers in early pregnancy. Infections also can occur after the delivery of the baby leading to blood infection and maternal death.
A pregnant woman must be taken to the nearest hospital for examination to prevent such infections.
