 While TB has been around for centuries in Sri Lanka, this treatable and curable disease once raging like wildfire in Sri lanka is now a disease of a bygone era. Cost effective simple treatments and interventions by the Health Ministry and the National TB Campaign saw a sharp plunge in this infectious disease caused by a bacillus.
While TB has been around for centuries in Sri Lanka, this treatable and curable disease once raging like wildfire in Sri lanka is now a disease of a bygone era. Cost effective simple treatments and interventions by the Health Ministry and the National TB Campaign saw a sharp plunge in this infectious disease caused by a bacillus.
It was officially declared as a disease that is no longer a threat to human life in Sri Lanka. Today, only a few new cases are reported from various parts of the country These pockets of resistance are the single biggest challenge that respiratory and chest experts face today.
According to them although the treatment is free for all patients attending clinics at state hospitals, getting them to follow through the treatment regimen to conclusion is the main problem.
Patients who don’t follow through treatment to the end can spread the disease to close contacts through nasal droplets, warns, Badulla Provincial Hospital Consultant Respiratory Physician Dr Neranjan Dissanayake.
Last week on our health page he spoke of how TB is spread and the causes.
Today, he talks of the challenges overcoming obstacles of new cases emerging in Sri Lanka.
Tuberculosis is a disease that has been with us for centuries. This treatable and curable disease still remains a major challenge in Sri Lanka.
Even though Sri Lanka has been categorised by the World Health Organization (WHO) as a moderate burdened country and is faring better than most of its neighbours in the South East Asian region we are yet to improve on the initial gains that were won.
The strong health infrastructure and the well trained human resources were instrumental in consolidating the current state.
The investigations and treatment is completely free for all patients who have been diagnosed with tuberculosis, with follow up being done to monitor complications and adherence to treatment.
The patients are usually given treatment under direct supervision by another person to prevent defaulting of treatment. Even though meticulous measures are implemented to control tuberculosis in Sri Lanka, there remains much to be done.
 Dr.Neranjan Dissanayake, Consultant Respiratory Physician, Provincial General Hospital,Badulla, last week on our health page spoke of tuberculosis and its many presentations. Today, he talks of the challenges of containing tuberculosis in Sri Lanka.
Dr.Neranjan Dissanayake, Consultant Respiratory Physician, Provincial General Hospital,Badulla, last week on our health page spoke of tuberculosis and its many presentations. Today, he talks of the challenges of containing tuberculosis in Sri Lanka.
Why do you say Tuberculosis is still a challenge in Sri Lanka?
In any disease, the aim of the health system is to eradicate it completely from the country. We have achieved it in many diseases. But, with regard to tuberculosis, we are far away from that point. According to the WHO, it is calculated that Sri Lanka is expected to have 14,000 new patients with tuberculosis each year. One in 1,000 of the population has tuberculosis.
We are successful in treating only 85% of the patients with tuberculosis and 6/100,000 patients die. A significant proportion of patients do not complete treatment risking their lives, as well as others. Even though the resistance of the bacteria to the standard anti tuberculosis drugs is minimal in Sri Lanka, and we have a low burden of HIV, I think we should be vigilant to this threat as well.
What specific areas would you identify as problems?
1. Delay in presentation and diagnosis: There is still a significant delay in diagnosing patients with tuberculosis. This delay will cause two main problems. One, is the destruction of the organ or system of the body due to tuberculosis. When this happens the scarring will be irreversible, causing permanent disability to the patient which may lead to death. The second, which I think is very important in the community, is the spread of the disease to another. Tuberculosis of the lung, with bacteria in the sputum will be spread from person to person very easily. But, treatment for about 2 to 4 weeks will usually make them non infective. So, every day delayed, there is an increased risk of another person being infected.
2. The missing 4,000: As I pointed out we should have 14,000 new patients diagnosed each year. But we diagnose only about 10,000. Hence, the rest is in our community. They will gradually deteriorate and some of them will be spreading the disease. Especially, among children, the detection rate is very low than what we expect.
3. Inability to reduce the death rate of tuberculosis: In any disease there are deaths. In tuberculosis, even though we have effective treatment, we have been unable to reduce the death rate, in patients who are diagnosed and are treated for tuberculosis.
4. The static treatment success rate: We strive to achieve 100% of treatment success in any disease. But, it might not be practical. In Sri Lanka our success rate is better than many of our neighbours, but still static at around 85%. A major concern is the discontinuation of treatment by the patient.
5. Double trouble: We have a significant proportion of patients with diabetes, kidney failure, smokers and drug abusers, liver disease among us. It has been proven that when you have a coexisting disease or habit, the treatment will get complicated and improvement delayed. Another important aspect is patients with psychological issues. This will invariably cause issues when treating.
Why is there a delay in diagnosis?
There are many aspects to this issue. People with symptoms suspected of tuberculosis not coming for treatment is a major problem. This is mostly due to a lack of awareness.
Referring patients with symptoms for simple tests, such as, examining a sample of phlegm is sometimes delayed. When the patient goes from one doctor to another, again, there will be a delay. In some areas of the country there is a lack of infra-structure and personnel, which may contribute to this. In complicated patients, the lack of advanced investigations will deter early diagnosis.
Where are the missing 4,000?
This actually is a calculated value derived from data. But, we are missing a significant proportion close to this value. Some probably have not sought treatment as I have mentioned above. Some might have not been diagnosed due to the above factors.
So, improving awareness among the general public and the medical profession is very important.
Why do people die of tuberculosis?
Tuberculosis is a devastating disease that scars the organ or system, making it dysfunctional.
Hence, it is very important to start treatment as early as possible. Some of the deaths are attributed to the delayed presentation for treatment.
When they are admitted, they already are in a very critical state. Some deaths might be due to the toxicity of the drugs, which need close monitoring. Some deaths can be attributed to a lack of intensive care and in ward facilities for TB patients, as in many wards there is a reluctance to manage these patients.
Other patients who die have multiple other diseases, such as, poorly controlled diabetes , kidney disease etc. I think the time is ripe to have dedicated wards for tuberculosis patients with adequate protection to the staff and facilities to the patients in at least District General Hospitals.
The reasons why we have not been able to improve on the treatment success rate?
I think we should be happy with the value of 85%. But, we should strive for at least 95%. Patients not taking treatment properly is a major issue. To prevent that, we have the DOTS strategy which we should strive to implement stringently. Many social and cultural issues affect this.
Lack of responsible people willing to provide drugs with supervision, difficulty in transport to a centre, poverty, lack of social support, working in a different area, psychological issues, are some. There should be a concentrated social effort to tackle these issues.
Do other diseases affect the control of tuberculosis?
Definitely. There is evidence to suggest that diabetes that is poorly controlled can increase the risk of having TB, and when treated, the bacteria remain in the body longer.
Kidney diseases and liver diseases make treatment very complicated, and difficult to treat. Fortunately, we do not have a lot of people with HIV(AIDS), but due to social changes and immigration this might change. Hence vigilance is important.
What other threats do you think that will affect TB control in Sri Lanka?
Workers and immigrants coming from most of our neighbouring countries and other countries have a high degree of drug resistant tuberculosis. Hence, I think we should have a proper mechanism of screening immigrants at entry points.
What is drug resistant Tuberculosis?
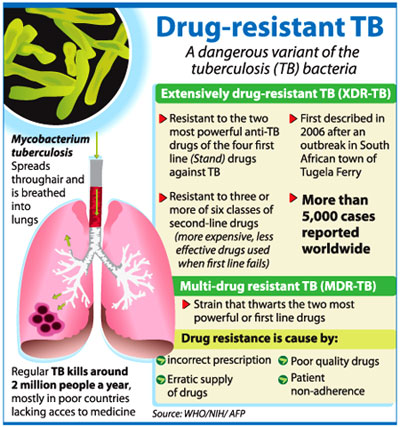
Tuberculosis is usually treated with a combination of four drugs; Rifampicin, Isoniazid, Ethambutol and Pyrazinamide. Of these Rifampicin and Isoniazid are the cornerstones in treatment. When the bacteria are not killed by a single drug we call it “mono resistant”.
If it is resistant to Rifampicin and Isoniazid, we call it Multi drug resistance (MDR), which is a dreaded condition, where treatment success rate is around 60% and is thrice as lengthy and 20 times more expensive to treat. In the world, bacteria has been isolated, that are resistant multiple drugs and sometimes all drugs.
This will be a major problem in future, in the world. At present, the rates in Sri Lanka are very low but we should not be complacent.
What will be the future of TB control in Sri Lanka
I think we have been successful overall in combating tuberculosis. But, there is much to be done.
I am happy that the Sri Lanka College of Pulmonogists and the Ministry of Health through the National Program to Control Tuberculosis and Chest Diseases , have taken some important steps to identify and rectify these problems. What we need is public support. “Please Help us to help you”.
Dr.Neranjan DissanayakeMBBS(SL),MD(Medicine),MRCP(UK),MRCP(London)Consultant Respiratory Physician.Respiratory Disease Treatment Unit & District Chest Clinic
